A patient walked into my clinic one afternoon holding his jaw, visibly distressed. He had been enjoying a routine lunch when he accidentally bit into a small stone hidden in the rice. The sharp crack he heard was not the stone. It was his tooth.
The pain was immediate, deep, and radiating. Biting became impossible. Even closing his mouth triggered discomfort. Situations like this are more common than we imagine, and they often lead to one question from patients: “Can this tooth be saved… or will I lose it?”

What Actually Happened?
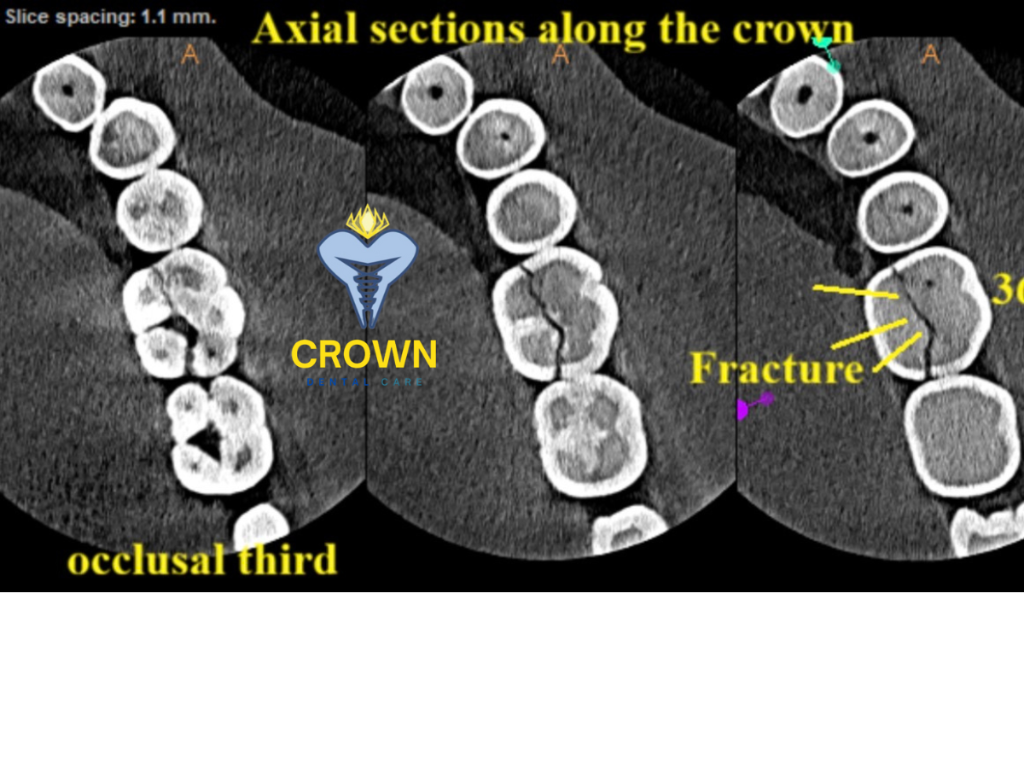
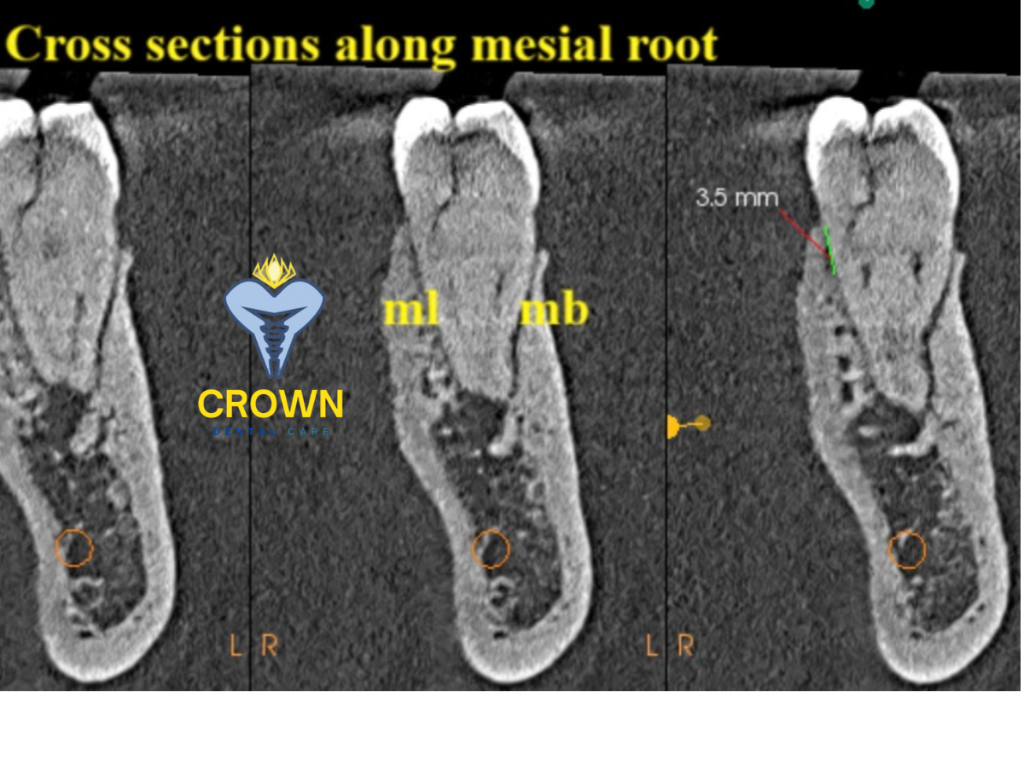
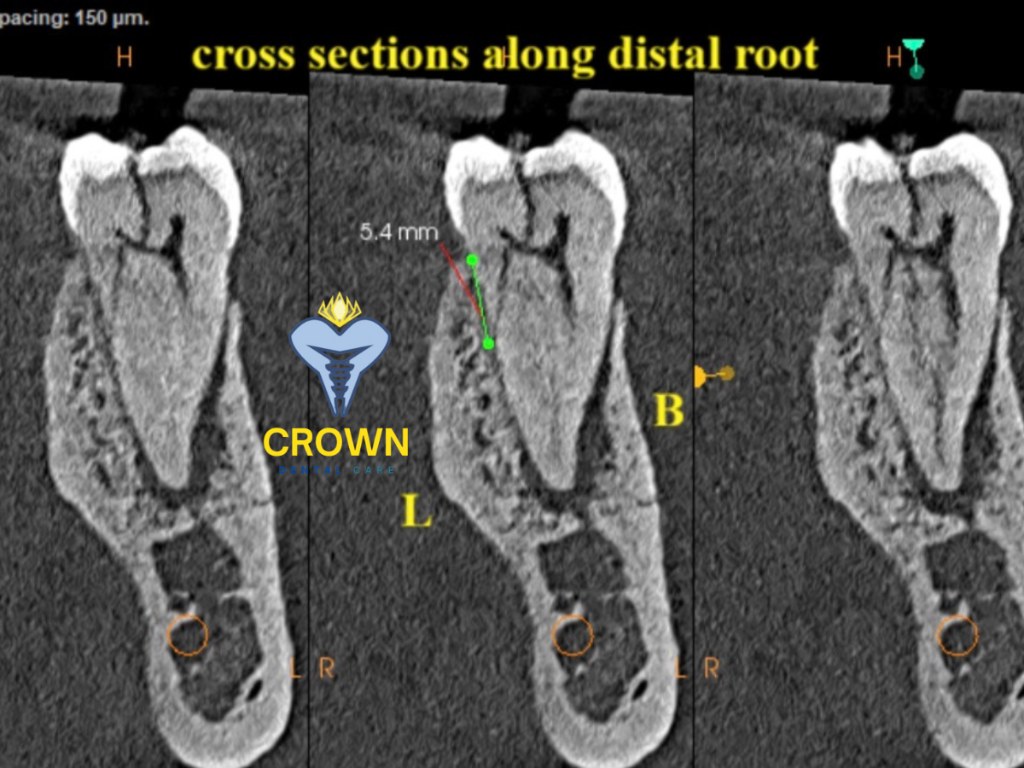
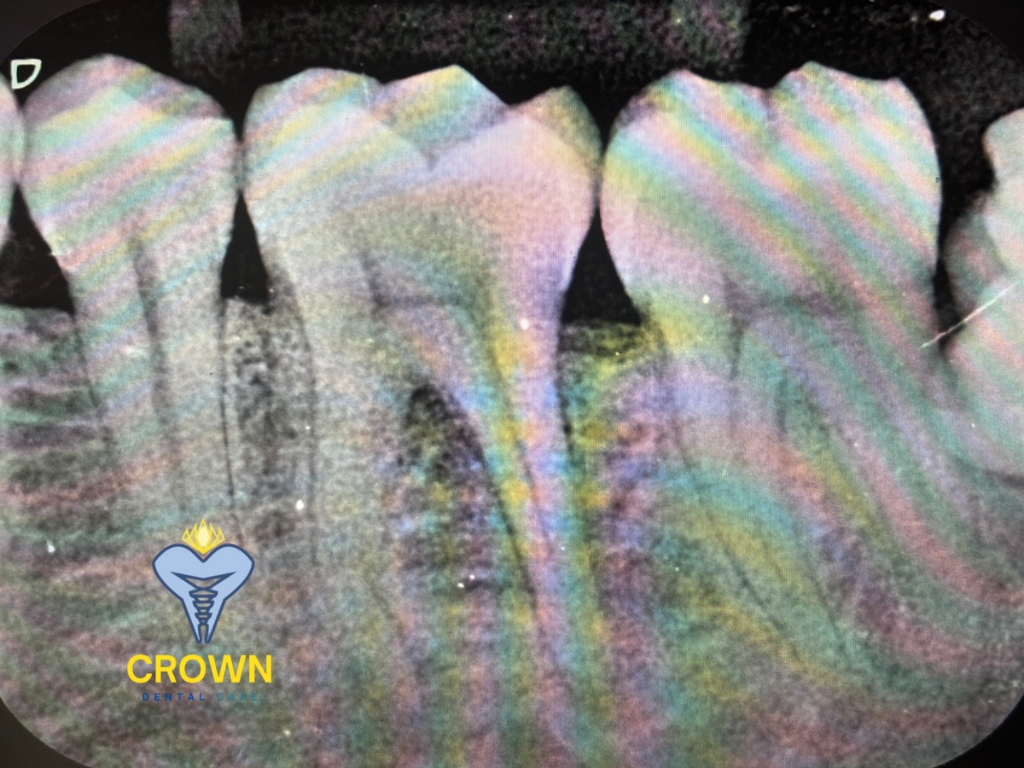
Clinical examination revealed a fractured molar. Radiographic imaging and CBCT cross-sections showed:
- A vertical crack extending through the crown
- Compromised tooth structure
- Risk of propagation into the root
- Localized bone still largely intact
In such cases, root canal therapy alone is rarely predictable. The structural integrity of the tooth is already compromised. Retaining it may only delay the inevitable and risk further bone loss.
This is where Immediate Extraction with Implant Placement becomes a powerful option.
What Is Immediate Implant Placement?
In simple words, it means: Removing the damaged tooth and placing a dental implant in the same appointment.
Instead of extracting the tooth and waiting 3–6 months for healing before inserting an implant, both steps are combined. The goal is not just speed, but preservation.
Preservation of:
- Bone volume
- Gum contour
- Natural smile architecture
- Patient confidence
Why Timing Matters
After a tooth is removed, the surrounding bone begins to shrink. Studies show:
- Up to 40% bone width loss can occur in the first 6 months.
- The most rapid resorption happens in the first 8–12 weeks.
- Soft tissue collapse follows bone loss, affecting esthetics and function.
Immediate implant placement acts like a placeholder. It tells the bone, “Stay here, you are still needed.”
What Patients Experience
From a patient’s perspective, the benefits are clear:
- Fewer surgical visits
- Reduced overall treatment time
- Better cosmetic outcome
- Faster return to normal chewing
- Psychological relief from “not having a missing tooth”
Pain perception is often lower than expected because the implant surgery is controlled and planned, unlike the sudden trauma that caused the fracture.
What Clinicians Evaluate Before Choosing Immediate Placement
Immediate implants are not a shortcut. They are a precision-driven decision. Key parameters include:
1. Bone Quality and Quantity
Minimum apical and circumferential bone required for primary stability. Ideal insertion torque often targeted between 30–45 Ncm.
2. Infection Status
Acute uncontrolled infection is a contraindication. Chronic localized lesions can still be managed with debridement and irrigation.
3. Socket Morphology
Intact socket walls increase predictability. Buccal plate thickness ideally ≥1.5–2 mm.
4. Soft Tissue Biotype
Thick gingival biotype favors esthetic success. Thin biotypes may require connective tissue grafting.
5. Occlusal Load
Immediate loading decisions depend on occlusal scheme and parafunctional habits.
Clinical Data Supporting Immediate Implants
Modern literature consistently reports:
- Survival rates between 94–98%, comparable to delayed implants.
- Marginal bone loss often <1 mm in the first year when protocols are followed.
- Improved papilla preservation and gingival contour stability in anterior zones.
However, these outcomes rely heavily on case selection and surgical precision.
The Role of Imaging
CBCT imaging is not a luxury here. It is a necessity. Cross-sectional views help visualize:
- Root morphology
- Bone density gradients
- Proximity to vital structures
- Hidden fractures
- Implant angulation planning
It transforms guesswork into geometry.
The Procedure in Brief
- Atraumatic Extraction: Preserve socket walls at all costs.
- Socket Debridement: Remove granulation tissue, irrigate thoroughly.
- Implant Placement: Engage apical or palatal bone for stability.
- Gap Management: Bone graft or biomaterial if jumping distance >2 mm.
- Temporary or Healing Cap: Based on primary stability and occlusal considerations.
When Immediate Implants Are Not Ideal
- Extensive bone destruction
- Vertical root fractures extending deep apically
- Uncontrolled systemic conditions
- Poor oral hygiene or compliance
- Heavy bruxism without management
In such cases, staged treatment remains safer.
The Human Side of It
For the patient who bit into that stone, the decision was clear. The tooth was beyond restoration, but the surrounding bone was strong. Immediate implant placement allowed him to leave the clinic not with a gap, but with a plan and a solution already in motion.
Pain was addressed. Structure was restored. Confidence returned quickly.
Final Thought
Immediate extraction and implant placement is not merely about speed. It is about respecting biology while using technology wisely.
For patients, it means fewer interruptions to daily life. For clinicians, it demands meticulous planning, imaging, and execution.
When done right, it converts an accident into an opportunity for long-term oral stability.